Can People with Heart Disease Exercise Safely?
Staying active is essential for the heart and overall health. Regular activity is one of the best ways to make a good recovery once diagnosed or treated for heart disease. But how, and how much?
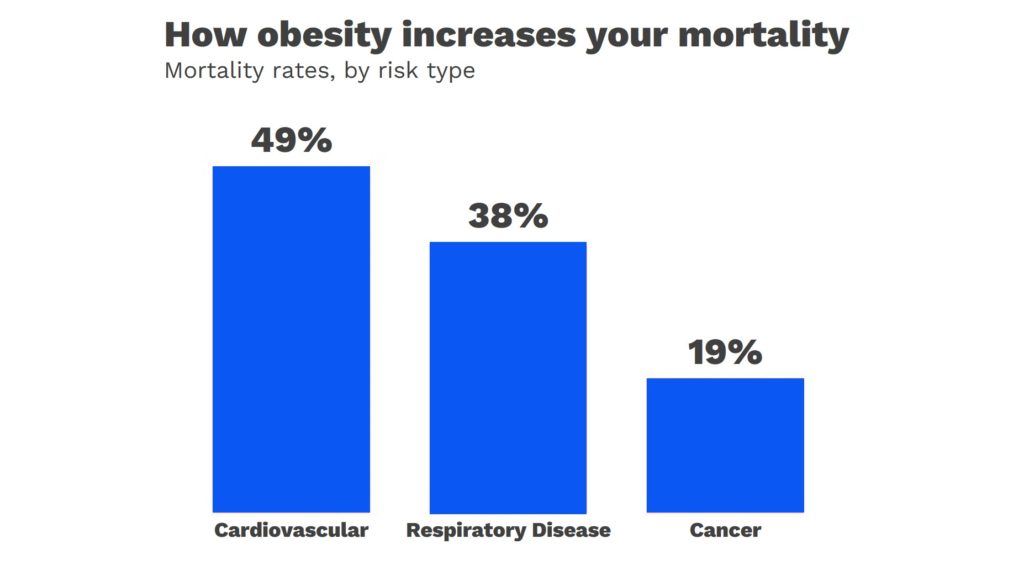
A regular exercise is one of the most important things you can do for you heart. Being active helps you live longer and reduces the risk of heart disease by 50%. But once you are diagnosed with heart disease, you may be scared and feel uncertain as where do you start? And how much physical activity is healthy and safe?
In this blog we will try to explain why and how even people whose conditions put them at higher risk of cardiac arrest can exercise safely. Even in patients with damaged heart that are causing heart failure, exercise can be important for improving quality of life. But this has to be within reason and care should be taken to avoid worsening the underlying conditions.
What should people consider when exercising with a heart condition?
Most importantly the underlying heart condition should be considered while developing an exercise plan.
example
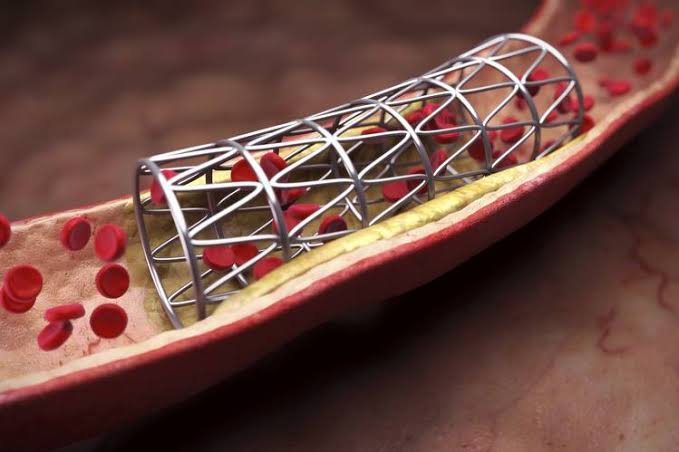
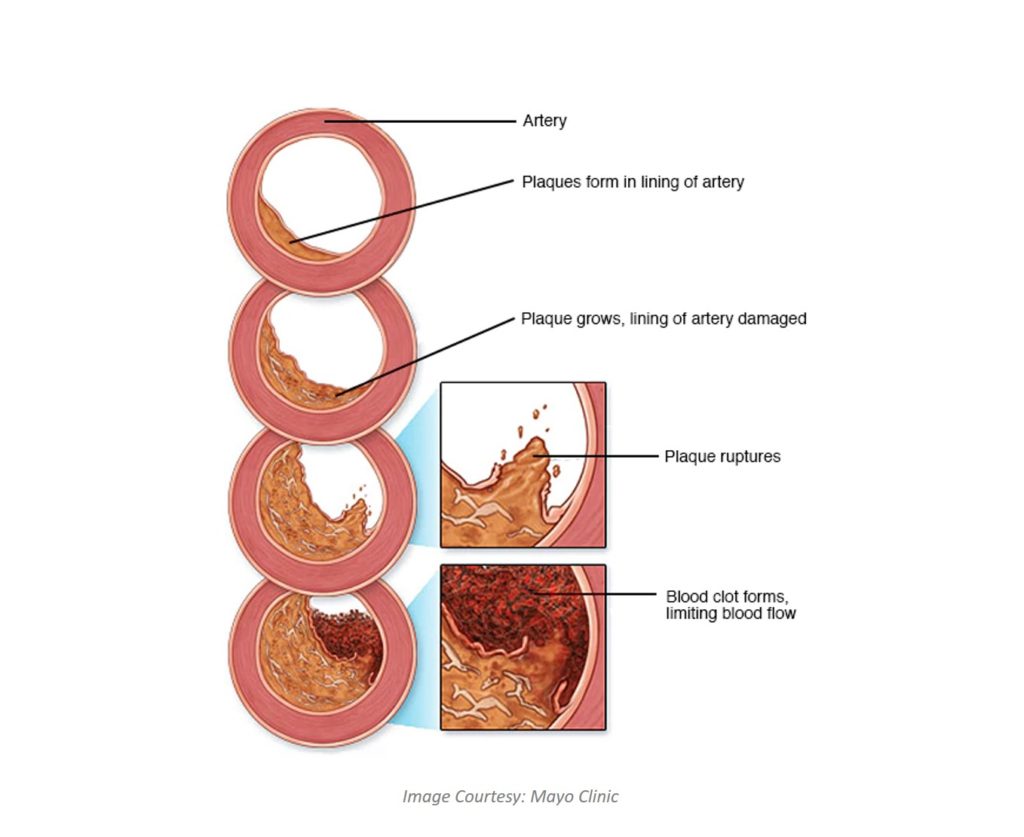
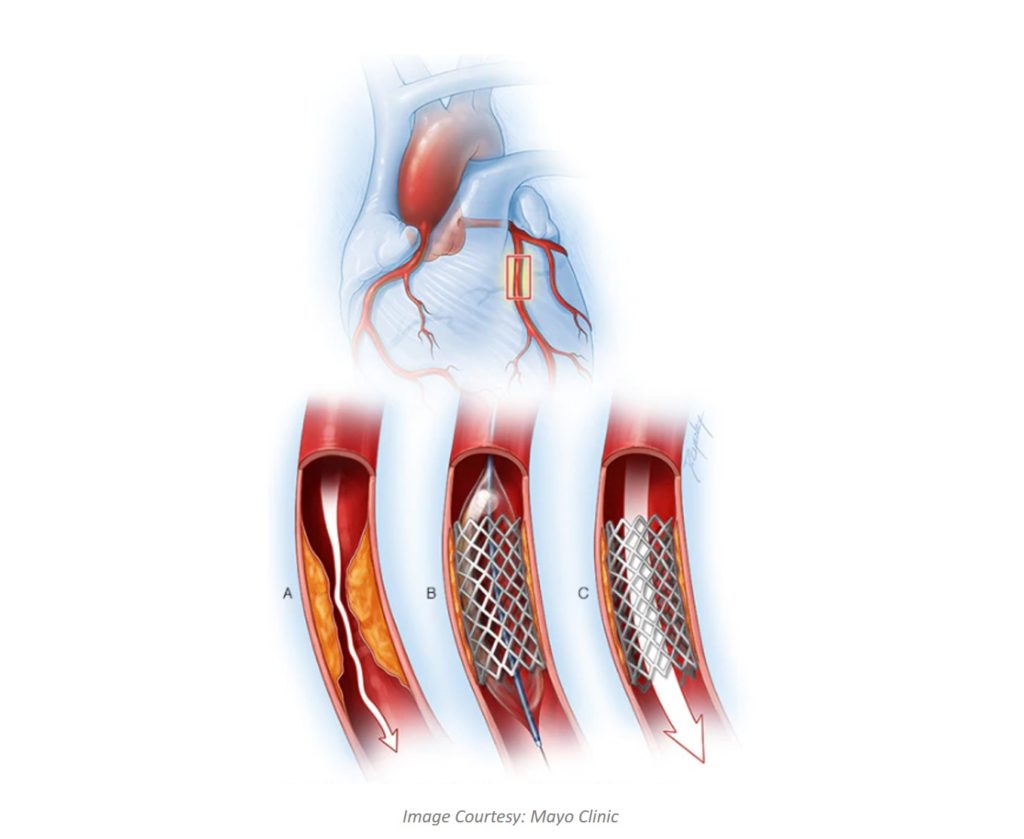
If someone has coronary artery disease (blockage, of the arteries due to cholesterol), then overexercising may cause chest pain and increases the risk from the underlying conditions.
On the other hand, patient with heart rhythm problems, may exercise as much as they wish.
What type of exercise is usually advised? Does it exclude cardio?
Heart disease patients can do cardio exercise and is indeed good for the prognosis. But the intensity of cardio exercise must be tailored and planned by the cardiologist according the patient’s condition.
In general, if your health condition is negatively impacted by exercise, high-intensity or competitive sports should be avoided. Taking a personalized approach from your cardiologist is advised.
What are the warning signs to take care of while exercising?
Key to minimize the risk is to avoid excessively intense exercise or competitive sports. If you or the patients have breathlessness, chest pain, palpitations or dizziness during exercise, one should stop exercising immediately and seek medical from cardiologist nearby.
Wrapping Up…
Physical activity is good for everyone with heart disease and even small amounts are beneficial. The best way to know if you are doing an exercise properly is to “listen to your body” and notice any warning signs as mentioned above. We hope these guidelines & tips will help heart patients and their health professionals choose the best and most enjoyable activities for them.





Recent Comments